Your teeth provide a detailed account of your life, much as a tree's rings record its history, a groundbreaking study shows.
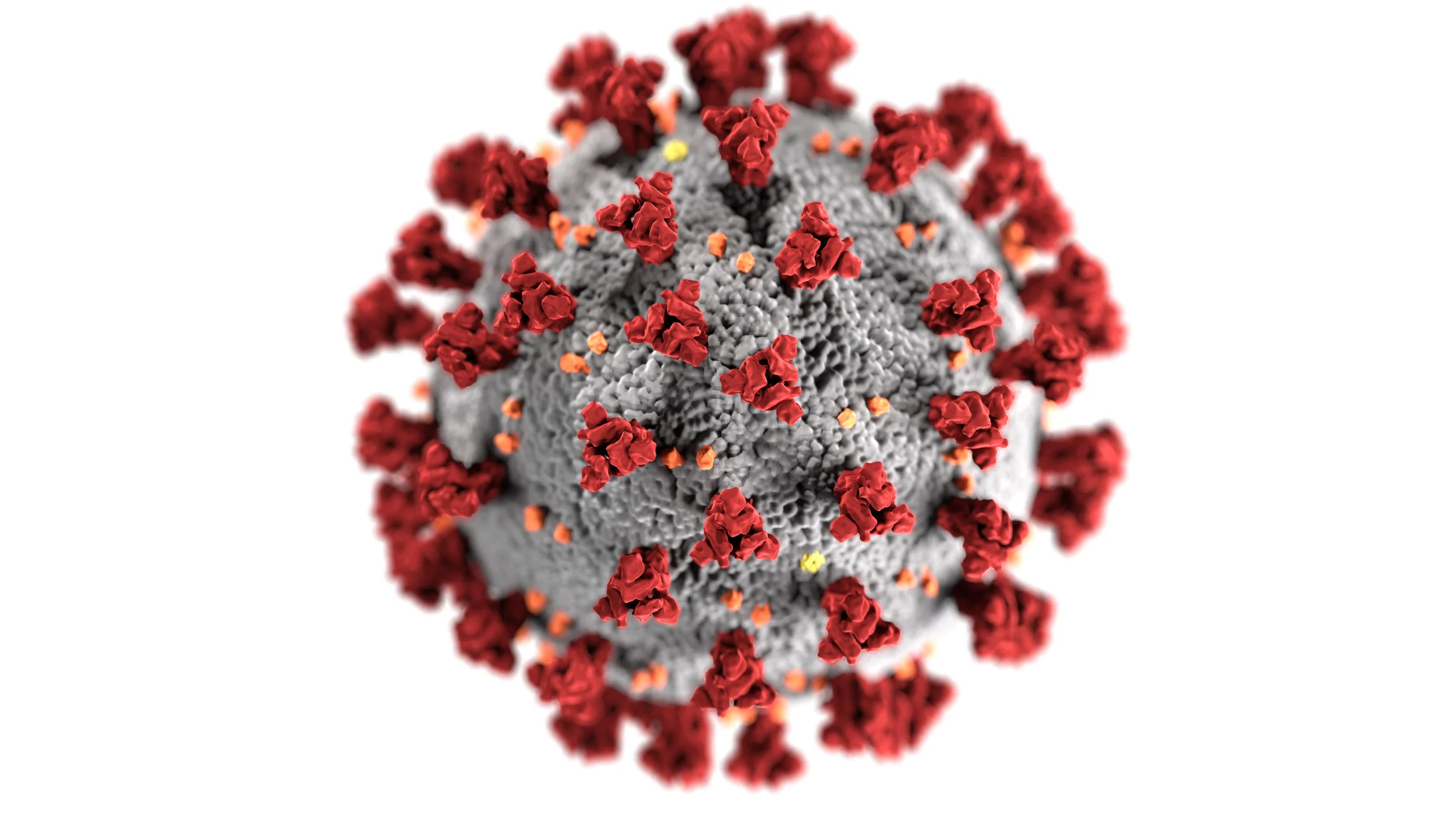
Donate to help support healthcare Workers
Please help support our local healthcare workers with Protective equipment so that they in turn can safely provide much-needed medical care to our fellow citizens affected with Covid-19 in the coming days and weeks.
NO DONATION IS TOO SMALL!!
Some NEEDED items from COMMUNITY RESIDENTS include,
• Any type of face mask and N 95 face mask
•Safety goggles
•Latex and non Latex Gloves
•Hand Sanitizers >60% alcohol concentration
•Antibacterial soap
NEEDED ITEMS FROM HEALTHCARE PROFESSIONALS
• Procedure masks
•Isolation gowns
•N 95 mask
•Surgical mask and gowns
•Face shield and goggles
Another Vaping Hazard: Less-Healthy Mouths
How to Avoid Stained Teeth When You Enjoy Red Wine
Brush Your Teeth To Protect The Heart
Dentists Already Are Prepared for the Coronavirus
Special sensory cells in gums protect against periodontitis
Periodontitis is a serious gum disorder induced by an imbalance in the bacteria and other microorganisms of the mouth (the oral microbiome). It is the sixth-most prevalent infectious disease and the most common cause of tooth loss worldwide.
Monell Center Director and President Robert Margolskee, MD, PhD and cell biologist Marco Tizzano, PhD, along with colleagues from Sichuan University, found that the newly identified cells, known as solitary chemosensory cells (SCCs), are present in the gums of mice. Here they express several types of taste receptors along with a downstream coupling protein called gustducin. SCCs are taste-like chemical detectors that sense irritants and bacteria, and biologists have found them throughout the gut, urinary tract, nasal cavities, and now in the gums.
"These sensory cells may provide a new approach for personalized treatment of periodontitis by harnessing a person's own innate immune system to regulate their oral microbiome," said Margolskee.
The team showed that knocking out taste-signaling molecules like gustducin or genetically removing gum SCCs in the mice leads to overgrowth of pathogenic oral bacteria and periodontitis. Conversely, stimulating bitter taste receptors in SCCs promotes the production of anti-microbial molecules.
Mice without gustducin in their SSCs have a more damaging set of microbes living in their mouths compared to normal mice, implying that the lack of gustducin disconnects the sentinel cells' molecular signal to other systems. Importantly, differences in the oral bacterial composition of the gustducin-less mice compared to normal mice occurred before any loss of bone in the gums, implying that differences in the oral microbiome could be used as a harbinger of disease.
Soft drinks found to be the crucial link between obesity and tooth wear
Temporomandibular Joint Dysfunction Symptoms Following Massage Therapy
Researchers have estimated that 65%–85% of Americans experience some symptoms of temporomandibular joint dysfunction (TMD) during their lives. This is perhaps owing to the fact that the temporomandibular joint (TMJ) is the most frequently used joint in the body, moving 2000–3000 times a day. TMD is a condition that encompasses several pathologies of the jaw and the muscles of mastication (chewing). Symptoms of TMD are most common in people between 15 and 45 years of age, and are more common in women than men by a ratio of 5:1. A triad of predisposition, tissue alteration (neuromuscular, skeletal, and dental), and stress sufficient to cause jaw clenching and/or bruxism is usually necessary to provoke TMD.
Symptoms of TMD vary from case to case, but common complaints include: spasm and/or pain in the head, jaw, neck, and shoulder muscles; headaches; earaches; jaw clicking or deviation; limited jaw opening; clenching or grinding of the teeth; and dizziness. Causes can include whiplash, bruxism, malocclusion, anxiety, stress, trigger points, and postural dysfunction.
It is important for patients to seek treatment because muscle contractures may develop and degeneration of the disc, condylar head and articular eminence may occur if not corrected. There are several approaches to the treatment of TMD. These treatment strategies are as diverse as the patients presenting the symptoms. Because each patient presents differently, he or she should be assessed and treated according to his or her distinct needs. Because most of the causes and conditions associated with TMD are irremediable, it has been suggested that treatment be aimed toward symptomatic relief and not cures. Common treatment options include: splint therapy, occlusal adjustment, analgesic medications, surgery, acupuncture, trigger point injections, hydrotherapy, therapeutic ultrasound, electromyopathy, hypnorelaxation, cognitive-behavioral therapy, massage therapy, stress management, and biofeedback. Home care practices such as a soft food diet, a local application of ice, self-massage, hot showers, and stretching have also been suggested as being beneficial.
Treatments that are discussed in the dentistry literature focus on surgical repair, splint therapy, and medication. In addition, some dentists may choose to refer their patients to massage therapists to assist in treatment of this condition. Although support for the use of massage therapy as a part of a comprehensive treatment solution for TMD has been discussed, literature that addresses the effectiveness of massage therapy on TMD is limited and studies report varying degrees of success.
Botanical Drug Shows Effectiveness Against Head and Neck Cancers
A plant-based drug called APG-157 has shown signs of helping patients fight oral and oropharyngeal cancers, according to a phase I clinical trial led by the University of California at Los Angeles Jonsson Comprehensive Cancer Center.